USEFUL LINKS
Access to high-quality and timely local data is critical to improving the health of communities, providing them with the information needed to make the best decisions. These data inform policies and resource allocations at the state and local level, and can help strengthen the design and evaluation of interventions to meet specific community needs. They are also the basis for community health needs assessments that shape local health improvement plans.
An important source of health-related data at the local level are birth and death records, which are collected by the Texas Department of State Health Services (DSHS). Information included in birth records can be used to calculate maternal risk factors that impact the health of both mothers and their babies. These measures also offer a window into the health status of the entire community, as mothers are a subset of the larger population.
In order to increase the availability and accessibility of local data, UT System Population Health used the 2013-2015 Texas birth records to generate ZIP-code-level measures of three maternal risk factors: pre-pregnancy obesity, smoking during pregnancy, and prenatal care utilization. Each of the measures was calculated by year at the ZIP-code-level for ZIP codes with at least 100 births in that year. These measures were also calculated by racial/ethnic subpopulations for ZIP code areas with at least 100 births to mothers of that racial/ethnic group.
Prior studies suggest that birth certificates are a good data source for these three maternal risk factors. Year-to-year comparisons showed that each measure was stable across years. However, data users should be aware that birth certificates are known to contain errors that impact the accuracy of derived measures.
Data for all three years by race/ethnicity are provided in downloadable files, and 2015 data are presented in an interactive map on the UT System Population Health website. The pdf document provides summary descriptions of each measure for 2015, details on the data source, and definitions of each measure.
This project is the second of a series of local area data projects by UT System Population Health. The first project provided ZIP-code-level infant mortality rates for 2011-2014 (available at utsystempophealth.org/imr-texas) We hope these data are a useful resource for public health practictioners and researchers working to improve the health and wellbeing of all mothers and infants in Texas.
Obesity
One marker of a mother’s health as she becomes pregnant is her pre-pregnancy body mass index (BMI). A woman in the obese range of BMI when becoming pregnant is at an increased risk for a variety of maternal and fetal complications, including preeclampsia, gestational diabetes, congenital anomalies, and fetal death.
The local variation in pre-pregnancy obesity is dramatic across the state. In 2015, the prevalence of pre-pregnancy obesity in some ZIP codes was less than 10% while in others it was more than 40% (Figure 1). While pre-pregnancy morbid obesity is less common and shows less variability, in 2015 the prevalence was more than 10% in some Texas ZIP codes (Figure 1).
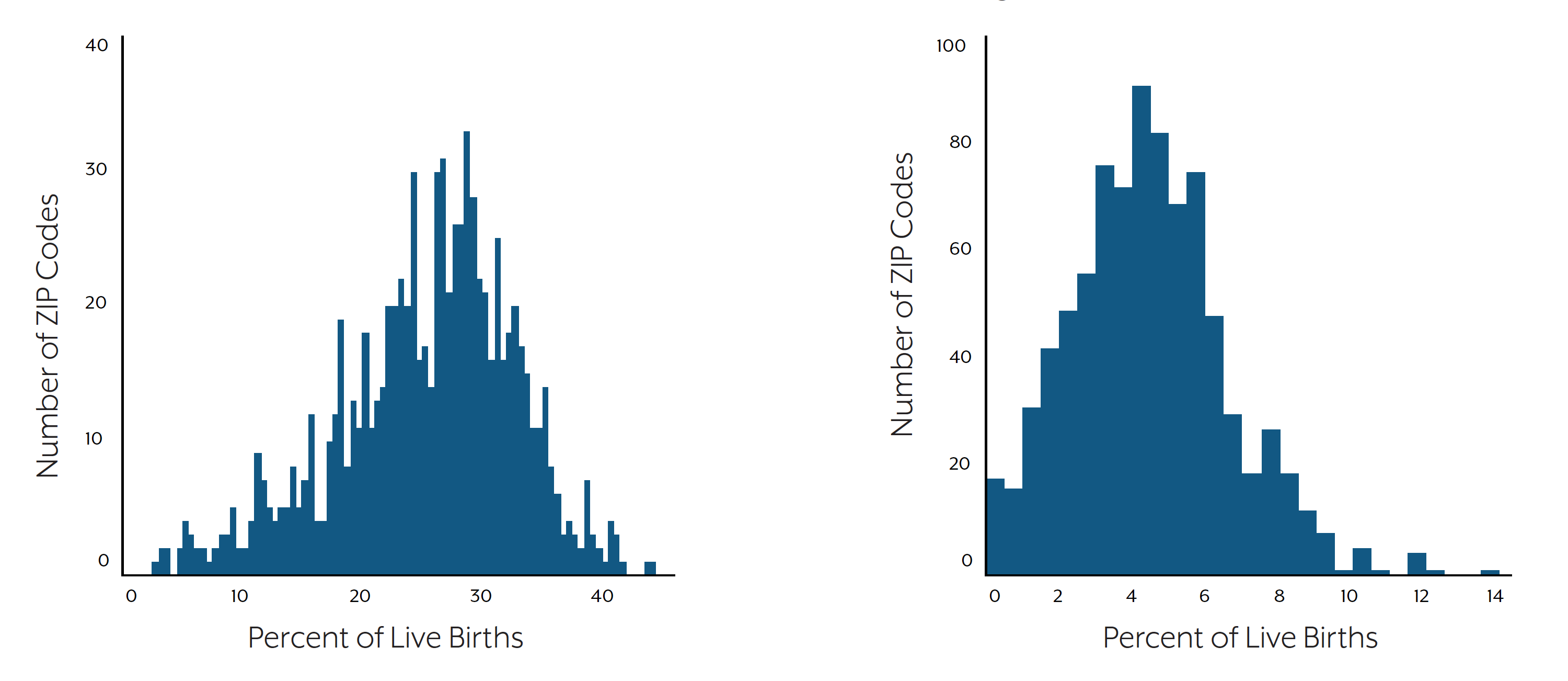
Left: Distribution of ZIP-Code-Level Percentages of Live Births to Mothers Who Were Obese Pre-Pregnancy: Texas (2015)
Right: Distribution of ZIP-Code-Level Percentages of Live Births to Mothers Who Were Morbidly Obese Pre-Pregnancy: Texas (2015)
Figure 1 illustrates one example of local variation of pre-pregnancy morbid obesity prevalence. Within ZIP codes with at least 100 births to Hispanic mothers in 2015 in Bexar County, the percent of live births to Hispanic women who were classified as morbidly obese prior to becoming pregnant ranged from a low of 1.1% to a high of 9.3%.
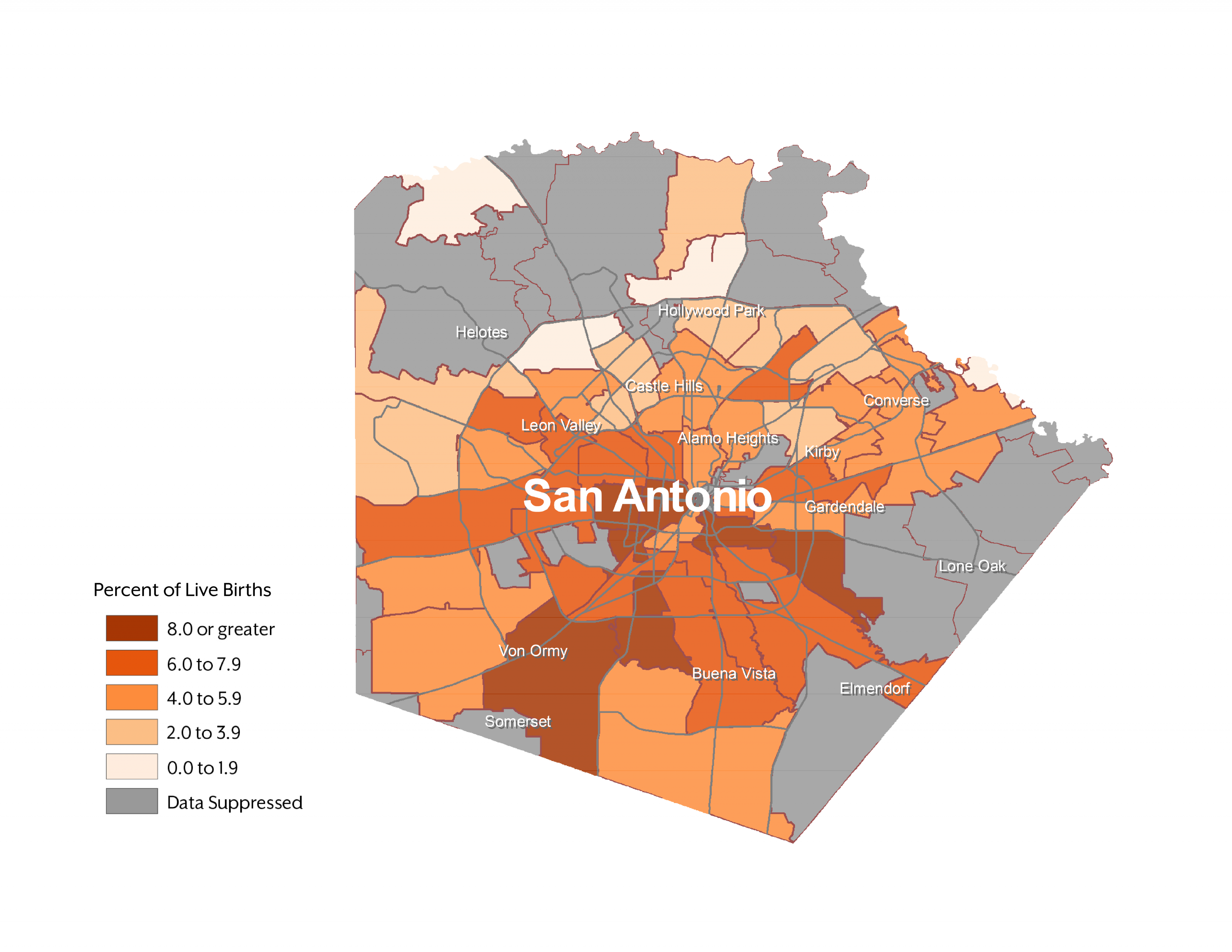
Figure 1. Percent of Live Births to Hispanic Mothers Who Were Morbidly Obese Pre-Pregnancy: Bexar County, Texas (2015)
Smoking
Smoking during pregnancy has important effects on fetal growth and long-term health. Smoking during pregnancy increases the risk of low birth weight, preterm birth, and certain birth defects, and may increase a child’s risk of obesity, asthma, and high blood pressure later in life.
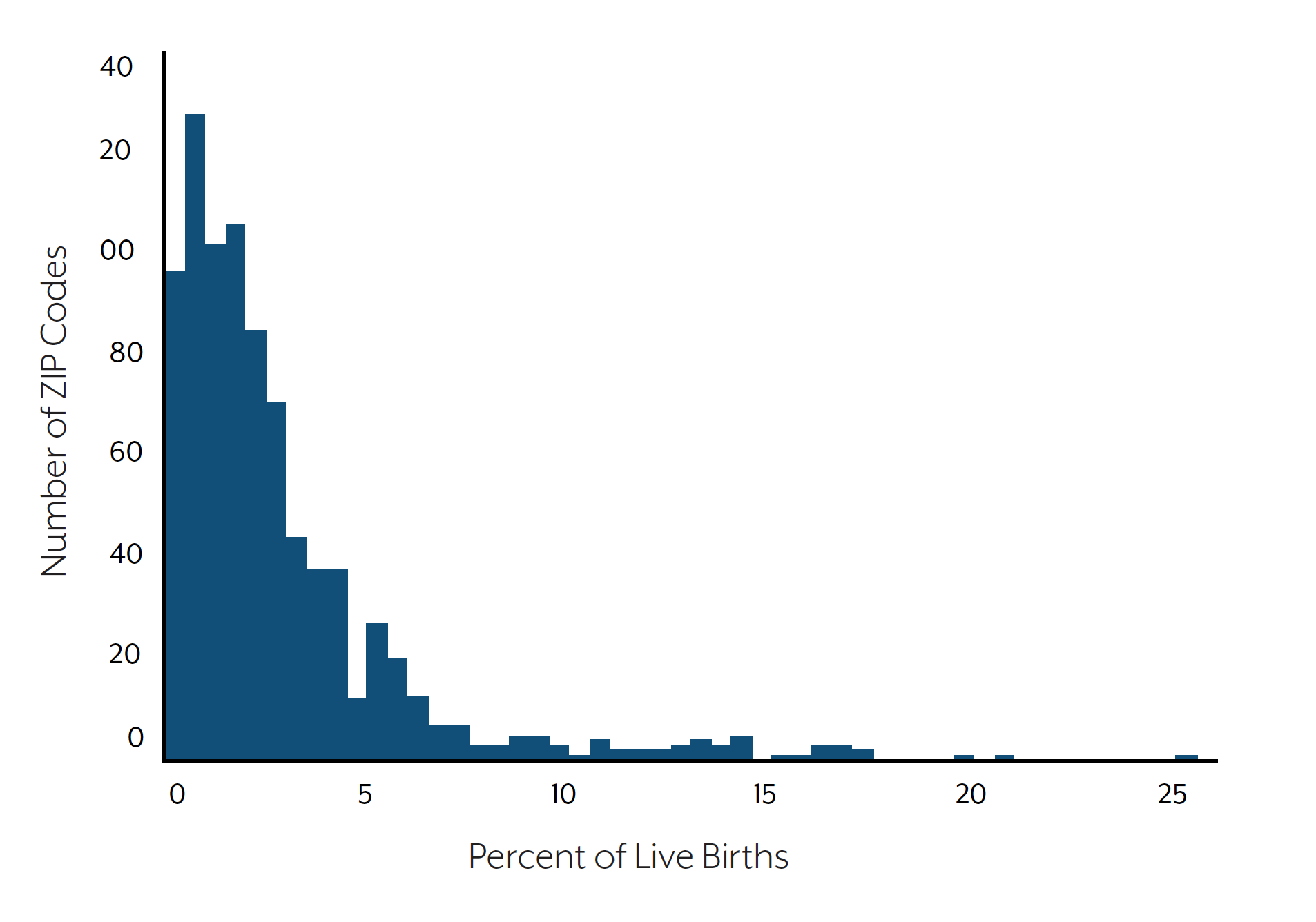
According to the National Center for Health Statistics, the percentage of women who smoked during pregnancy in Texas in 2016 was one of the lowest in the country.3 In 2015, over 30% of ZIP codes with at least 100 births met the Healthy People 2020 target of no more than 1.4% of pregnant women smoking during their pregnancy. An additional 48% of ZIP codes had a prevalence of smoking during pregnancy that was lower than the 2016 national prevalence of 7.2%.3 However, in 12% of the included ZIP codes, more than 10% of infants born were exposed to prenatal maternal smoking.
Distribution of ZIP-Code-Level Percentages of Live Births to Mothers Who Smoked During Pregnancy
Figure 2 illustrates one example of local variation in the prevalence of smoking during pregnancy. Within ZIP codes with at least 100 births to white mothers in 2015 in the Dallas/Fort Worth metropolitan area, the percent of live births to white women who smoked during pregnancy ranged from a low of 0.0% to a high of 25.5%.
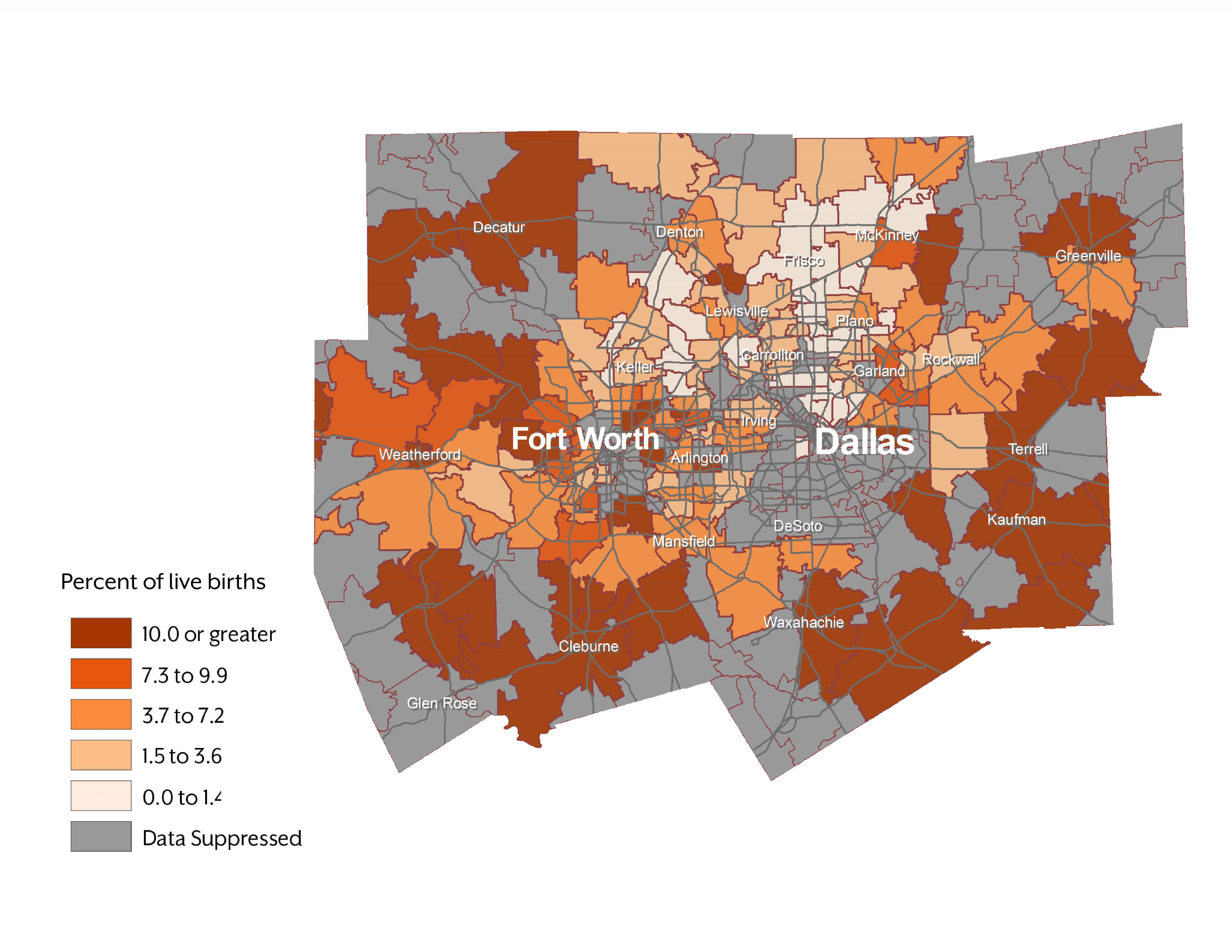
Figure 2. Percent of Live Births to White Mothers Who Smoked During Pregnancy: Dallas/Fort Worth Metropolitan Area, Texas (2015)
No Prenatal Care
Prenatal care is important to the health of the mother and the baby. During these visits, women with chronic health conditions or complications during pregnancy can be medically managed to reduce the negative outcomes for the baby. Inadequate prenatal care utilization increases risk of prematurity, neonatal death, and infant death.¹
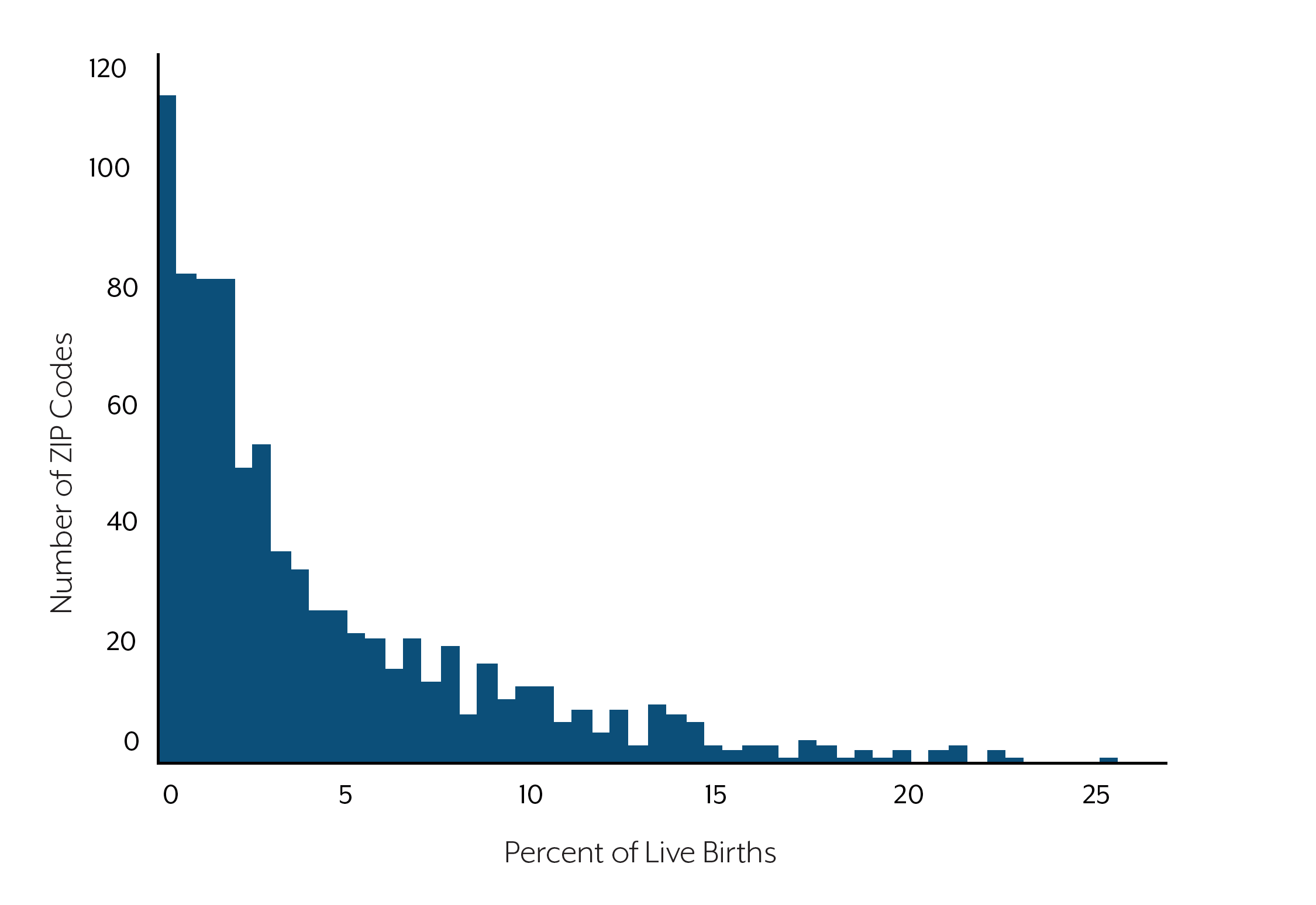
In half of the ZIP codes in the state with at least 100 births in 2015, fewer than 2% of infants’ mothers had no documented prenatal care. In 5% of ZIP codes, however, more than 10% of births in 2015 were to a mother who had not received prenatal care (Figure 5).
Distribution of ZIP-Code-Level Percentages of Live Births to Mothers With no Reported Prenatal Care
Figure3 illustrates one example of local variation in prenatal care utilization. Within ZIP codes with at least 100 births to black mothers in 2015 in Harris County, the percent of live births to black women with no reported prenatal care during their pregnancy ranged from a low of 0.0% to a high of 10.1%.
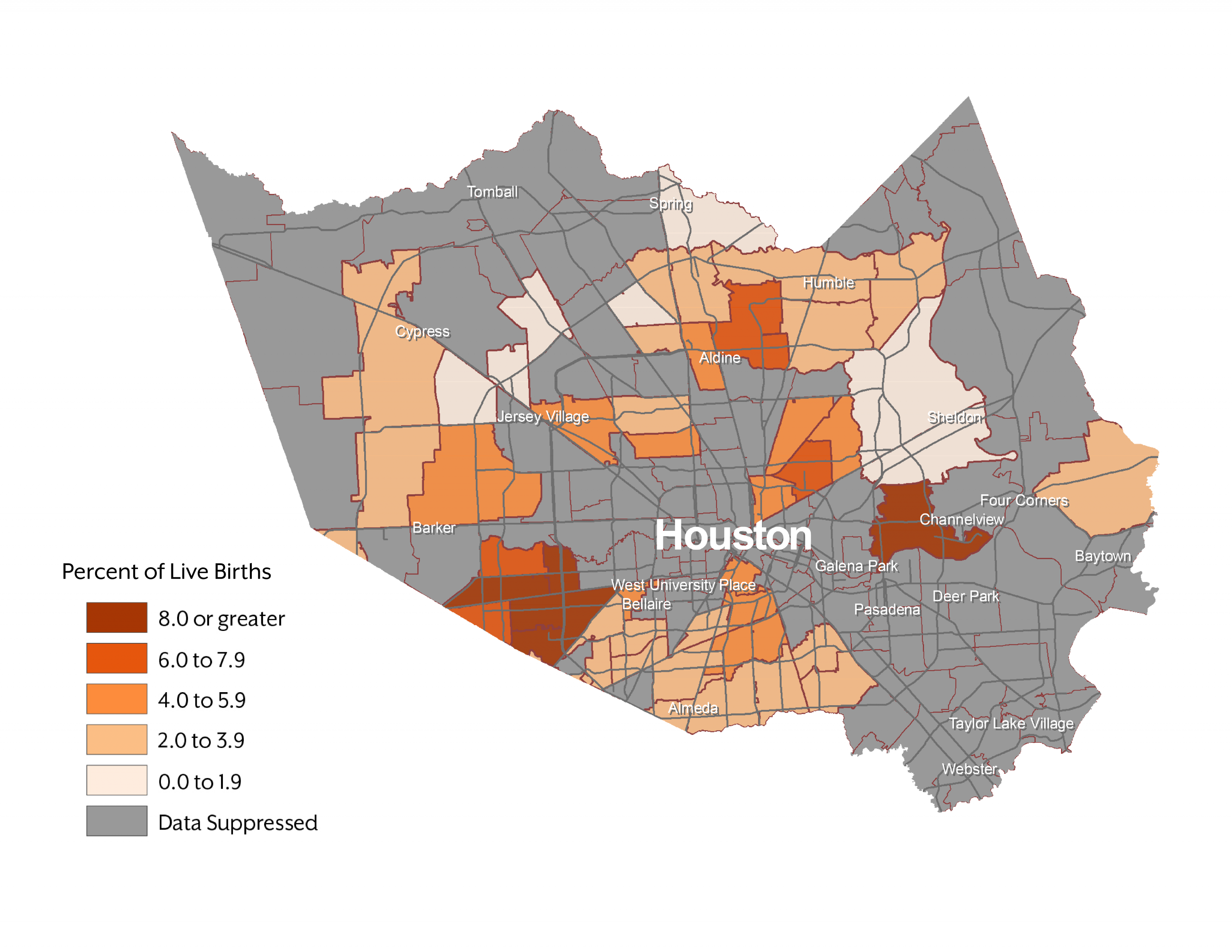
Figure 3. Percent of Live Births to Black Mothers With No Reported Prenatal Care: Harris County, Texas (2015)
Data Source
All measures were calculated using birth records provided by the Texas Department of State Health Services (DSHS). The dataset only includes live births that occurred in Texas to a woman who was a Texas resident. Live birth is defined as “the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of pregnancy, which, after such separation, breathes or shows any other evidence of life such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles, whether or not the umbilical cord has been cut or the placenta is attached; each product of such a birth is considered live born.”¹
Measure Definitions
Each measure is given as a percent of all live births during the specified year to mothers who resided in the ZIP code at the time of birth, excluding those with missing data for the specific measure. For measures by racial/ethnic subpopulations, only births to mothers of the specified racial/ethnic group are included in the denominator. Mother’s racial/ethnic category is categorized by DSHS, based on information on the birth certificate. In these categories, mothers with more than one race listed are included in the “other” category if they did not identify as Hispanic.
Pre-pregnancy obesity and morbid obesity
Pre-pregnancy obesity categories were assigned based on maternal age (in years) at delivery. For mothers ages 20 years old or older, body mass index (BMI) was calculated as pre-pregnancy weight in kilograms divided by height in meters squared; obesity was defined as BMI ≥ 30.0 and morbid obesity was defined as BMI ≥ 40.0. For mothers younger than 20 years old, BMI percentile for age and sex was calculated using the CDC standard growth charts for adolescents; obesity was defined as BMI percentile ≥ 95th BMI percentile for age and sex, and morbid obesity was defined as BMI percentile ≥ 120% of the 95th percentile for age and sex.
Smoking during pregnancy
Any smoking during any trimester of pregnancy reported on birth certificate.
No prenatal care visits
Zero prenatal care visits reported on birth certificate.
Data Suppression and Interpretation
In order to protect confidentiality and reduce spurious data variability, rates were suppressed for geographic areas with fewer than 100 births in a given year. This suppression rule was also applied to all of the race/ethnicity calculations. Therefore, rates by race/ethnicity are only available for ZIP codes with a large number of women in that racial/ethnic category.
Standard errors and 95% confidence intervals were calculated using a Poisson mean and the normal approximation method. All rates that survive the suppression rule but have a relative standard error of the rate (RSE) of 30% or greater were flagged as unstable in the dataset and on the maps. Flagged rates should be interpreted with caution.
Texas ZIP-code-level(a) Distribution of Maternal Risk Factors as Percentage of Live Births (2015)
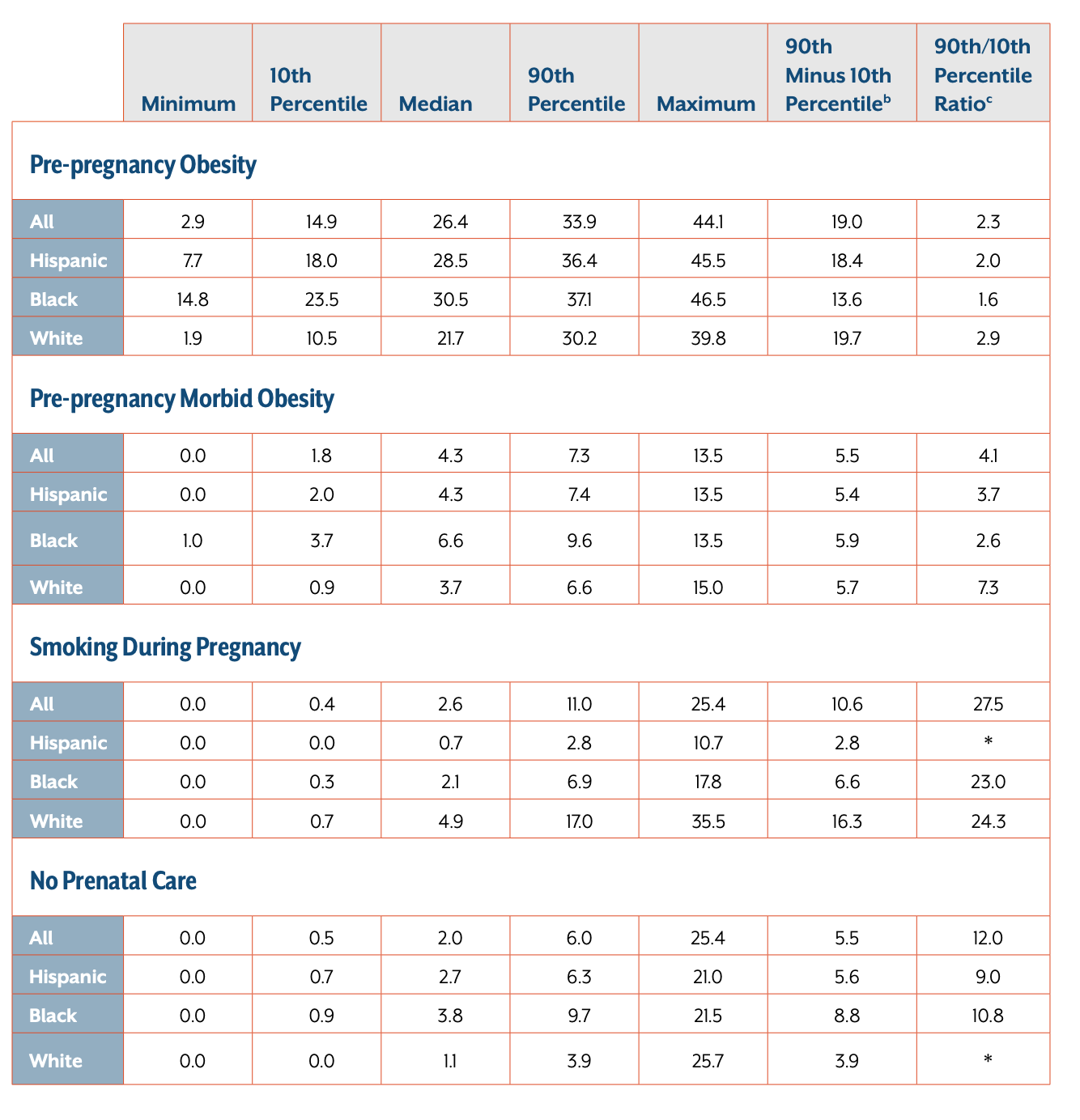
a Only ZIP codes with ≥100 births in 2015 are included. For prevalence measures by race/ethnicity, only ZIP codes with ≥100 births in 2015 to mothers in that racial/ethnic category are included.
b Measure of absolute geographic inequality.
c Measure of relative geographic inequality.
* Value cannot be calculated due to zero in denominator
See Technical Notes section for measure definitions.
Suggested citation: Nehme E, Mandell D, O’Neil M, Elerian N, Patel D, Karimifar M, Lakey D. (2018) Maternal Health Risk Factors in Communities Across Texas. Austin, TX: University of Texas Health Science Center at Tyler/University of Texas System.
